2 min read - Tachyarrhythmias
A 32 years old previously healthy male patient admitted with a history of palpitations for 1 hour duration. He had experienced a similar episode a few months back which lasted only for few minutes.
What are your concerns?
What are your concerns?
- First priority is to make sure that the patient is stable.
- Who is unstable?
- Hypotensive patient (Systolic BP < 90mmHg)
- Coronary ischemia (Ischemic chest pain)
- Cardiac failure (Patient has SOB)
- Patient with brain hypoperfusion (reduced conscious level)
IF ANY OF ABOVE ARE PRESENT IRRESPECTIVE OF THE TYPE OF ARRHYTHMIA YOU WILL HAVE TO PERFORM DC CARDIOVERSION (SHOCK)
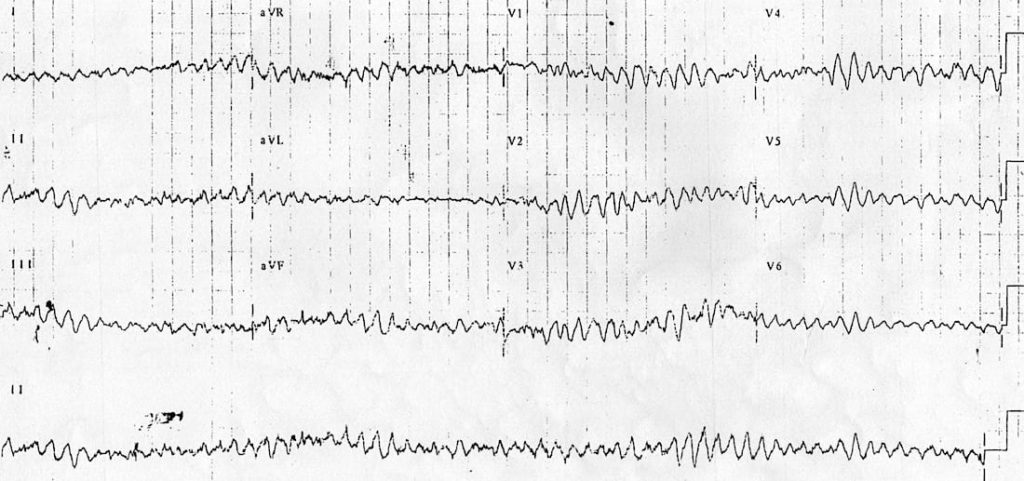
ECG
- Analysing tachyarrhythmias is a long topic, which might bore you.
- Let's learn a few short cuts to diagnose common arrhythmias.
- Look at the QRS
- Is it narrow or broad?
- Narrow complex tachycardias we usually encounter are
- SVT (Read and understand the proper nomenclature. SVT is a wrong term!)
- Atrial fibrillation/ flutter
- In most patients both are managed the same way.
- READ ABOUT THE OTHER NARROW COMPLEX TACHYCARDIAS.
- Broad complex tachycardias UNLESS PROVEN OTHERWISE ARE VENTRICULAR TACHYCARDIAS
- However some 'supra' ventricular tachycardias can mimic ventricular tachycardias
- Eg: SVT with a bundle branch block.
- Is it regular or irregular
- Regular narrow complex tachycardia = SVT
- Irregular narrow complex tachycardia = Atrial Fibrillation/ flutter
- Regular broad complex tachycardia = VT
- Irregular broad complex tachycardia = Ventricular Fibrillation
- However, as you start to learn more and more about ECGs you will realize that this is oversimplified and there are so many other arrhythmias in each category.
- REMEMBER, THIS IS ONLY A SURVIVAL GUIDE!
 |
| Diagnosis?? |
- I repeat, irrespective of the type of arrhythmia if the patient is unstable - SHOCK
- If the patient is stable
- SVT
- Perform vagal manouvers
- Medications
- Drug of choice is adenosine
- Contraindication is ASTHMA
- Give IV 6mg bolus (FAST) followed by a 10-20ml saline flush.
- patient will respond in a few seconds
- If it fails, you may try about two boluses of 12mg.
- However in the case of a SVT, even if the patient is unstable you may try adenosine as it's response is very very fast!
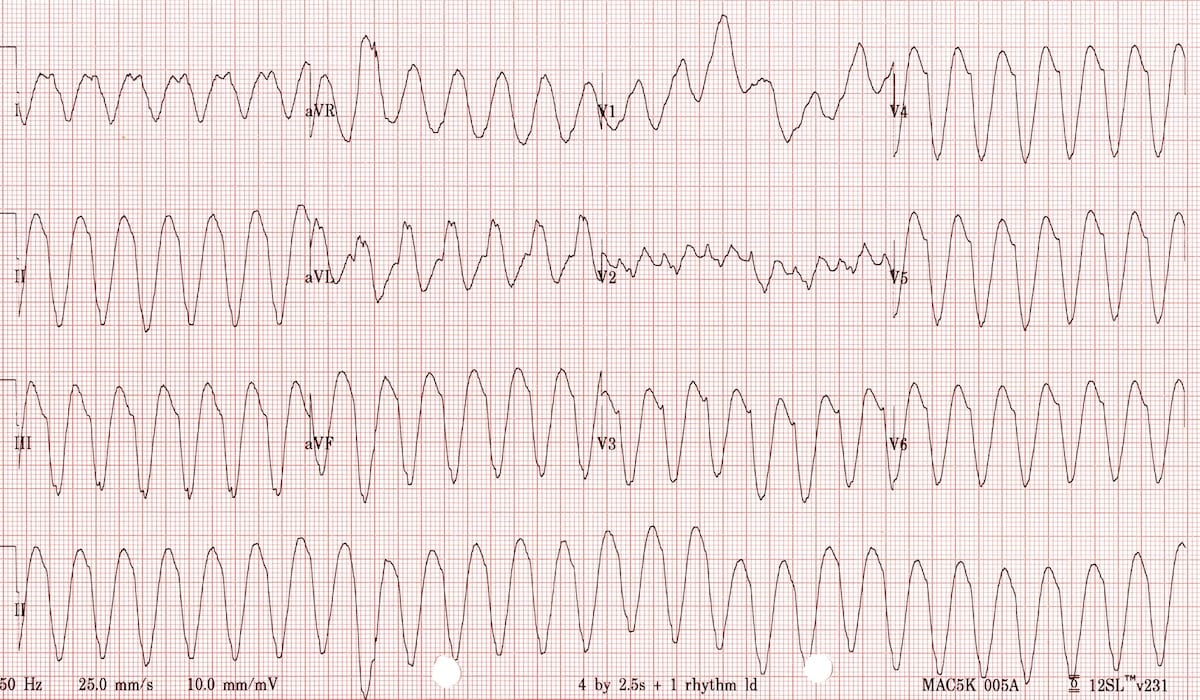
 |
| See the response to adenosine! |
- ATRIAL FIBRILLATION
- This is kind of complicated!
- We shall discuss it on a separate day.
- VENTRICULAR TACHYCARDIA
- Most patients will require SHOCK
- If the patient is stable you may try medications
- Amiadarone
- 150mg over 10 minutes
- Followed by 1mg/min infusion
- Lidocaine
- 1-1.5mg/kg bolus
- you may repeat up to a total cumulative dose of 3mg/kg every 5-10 minutes
- VENTRICULAR FIBRILLATION
- Homework
- What medications can you give for a patient who is hemodynamically stable with a VF??
Few facts about SHOCK
- Don't EVER shock yourself or your colleagues while attempting to shock the patient!
- Sedate the patient!
- Widely used medication is midazolam given as a bolus of 1-2.5mg
- Most of the defibrillators available are Biphasic
- Press the SYNC button for
- SVT
- VT
- AF
- NEVER FOR VF
- Energy level
- SVT 50-100
- AF 120-200
- VT 100
- VF - well, I guess you know what to give.
Vagal manouvers
- Avoid carotid massage in older patients
- You might give them a stroke!
- Modified valsalva manouver
- Read and check on youtube!
- Diving reflex
What if there is no response?
- Consider following
- Metabolic causes such as
- Electrolyte abnormalities
- Thyrotoxicosis
- Acidosis
- Hypo/Hyperglycemia
- Hypo/hyperthermia
- Toxins
- MI/ Pulmonary embolism
Isn't it too much for a day? Let's take a break.



Comments
Post a Comment